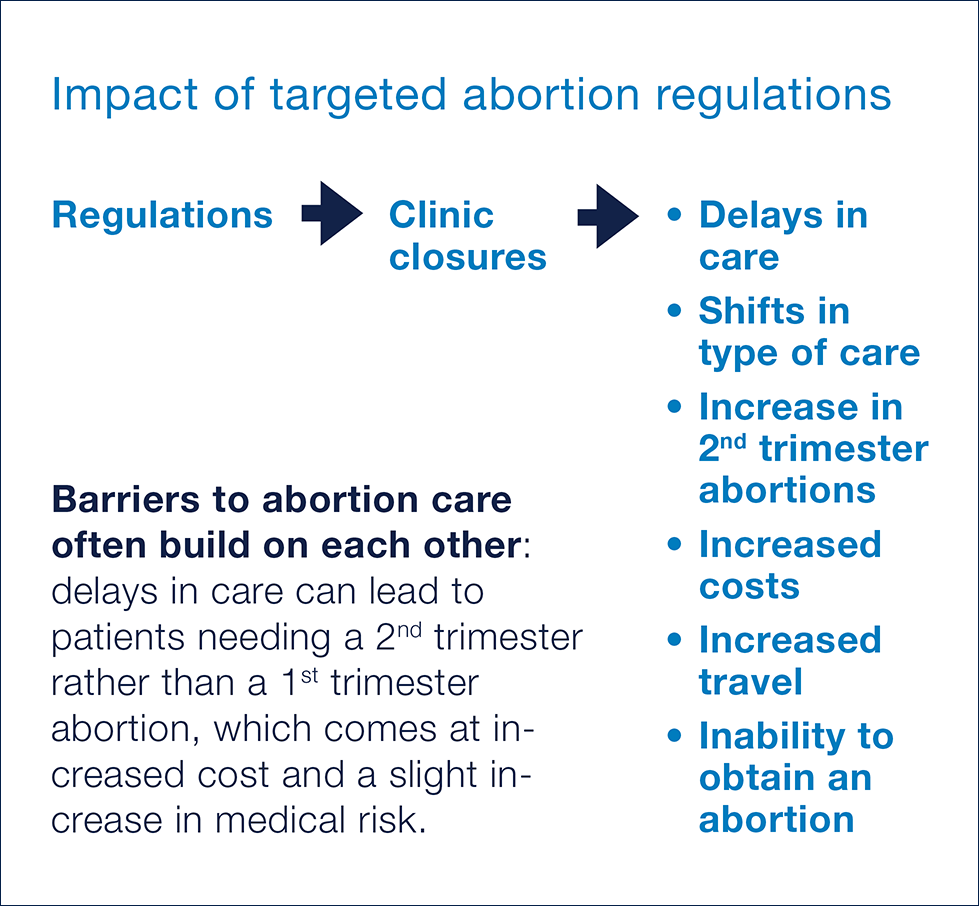
Many states have singled out abortion provision for stringent regulation, enacting more laws targeting abortion providers than laws governing other similar office-based procedures.1 Researchers analyzed the effect these laws have on abortion clinic operations, finding that they reduce the availability of abortion services and negatively impact patient experience.
Clinic Closures
Laws that regulate abortion clinics more stringently than facilities providing similar office-based procedures have led some clinics to close.2–4 For example, Texas’s law requiring abortion providers to maintain admitting privileges at nearby hospitals was likely the main contributor to the closure of 19 of the state’s 41 abortion clinics.5 Notably, these regulations do not increase patient safety.4, 6–7 Instead, they negatively impact patient experience in the following ways:
• Delays
When clinics close, demand increases at the remaining open clinics, leading to delays in patients being able to receive a timely abortion appointment.8 Patients may be forced to travel an additional 50 to 200 miles to reach an open facility, including traveling out of state, and they incur higher out of pocket expenses for their abortion, including extra days of childcare, lodging, and days of work missed.2–3, 5
• Changes in Care
Clinic closures create obstacles to obtaining a preferred abortion method. For some patients, this means having an aspiration abortion instead of a medication abortion, and for others, it means having an abortion in the second trimester instead of the first.9
Abortion is a very safe procedure, and abortion at any gestational stage is safer than childbirth.10 Yet the risk of complications from an abortion does increase later in pregnancy.11 Thus, experts agree that clinic closures may push some patients into having procedures that have a greater medical risk.12
• Increased Cost
Delays in seeking care and changes in care sometimes result in an increased cost of the abortion itself. Abortion is typically not covered by insurance, including Medicaid insurance, often due to state laws. Thus, patients typically pay for the abortion out-of-pocket.13 The average out-of-pocket cost of a first trimester abortion is $575, and for more than half of abortion patients, this is about one-third of their monthly income.14
Researchers describe the effect of increasing costs as a “negative feedback loop” in which the cost of an abortion increases as pregnancy progresses, and thus a delay in obtaining an abortion due to financial difficulty may result in a later, more expensive abortion procedure. This, in turn, may result in further delays, as patients try to raise the needed funds.15
Evidence-Based Bottom Line
The closure of abortion clinics due to targeted regulation increases barriers to and costs of obtaining care. In some cases, these barriers result in people not being able to obtain an abortion at all.
For more information:
References